Heat Disorders or Heat Related Illness
Every year during the hot summer season, we get to hear about quite a large number of people dying due to “heat wave” conditions in different geographical areas of the world. A much larger proportion of people suffer from less severe forms of heat disorders. 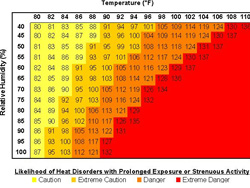 The incidence of heat related illness in a given areas can be correlated directly to the degree of rise of ambient temperature or more accurately by the Heat Index Chart , where the Air Temperature (in degree Fahrenheit) is plotted against the Relative Humidity (expressed as%).
The incidence of heat related illness in a given areas can be correlated directly to the degree of rise of ambient temperature or more accurately by the Heat Index Chart , where the Air Temperature (in degree Fahrenheit) is plotted against the Relative Humidity (expressed as%).
|
Heat Related Illness Results from:
|
|||
 |
|||
| Excessive Loss of Fluids and Electrolytes through | Inability to shed heat by circulating changes | ||
| Profuse perspiration | or by sweating | ||
 |
 |
||
| Body cannot compensate for losses | Temperature of inner core begins to rise | ||
 |
 |
||
| Dehydration |
Heat Stroke
|
||
 |
|||
| Heat Exhaustion, Cramps, Syncope | |||
What are the risk factors and who are vulnerable to Heat Related Illness?
The vulnerable group includes:
- The elderly and the children
- The physically and mentally disabled
- Alcoholics
- The chronically ill
- Those on drugs like neuroleptics and anticholinergic drugs etc
The risk factors include
- Geographical Factors
- Meteorological Factors
- Socio- economic and psychosocial factors
Three major forms of Heat illness are recognized.
 Heat Cramps: – Intense painful muscle cramps especially of lower limbs, sometimes of abdominal muscles. There is no elevation in core body temperature typically occur in young people exciting in hot weather. Also encountered in minor engaged in hard physical work in hot conditions with limited ventilation.
Heat Cramps: – Intense painful muscle cramps especially of lower limbs, sometimes of abdominal muscles. There is no elevation in core body temperature typically occur in young people exciting in hot weather. Also encountered in minor engaged in hard physical work in hot conditions with limited ventilation.
Related to depletion of sodium and other electrolytes with replacement of water but not salt
Treatment
- Discontinue exertion
- Replenish fluid volume with salted drinks
Heat Exhaustion:
Usually seen in individuals undertaking vigorous physical work in a hot environment. Factors that result in this syndrome:-
- A high work rate
- Extreme ambient temperature
- High relative humidity
- Inappropriate clothing
Characterised by the following:-
Elevation in core body temperature (37- 40 degree C)
Tiredness or fatigue
Muscular weakness
Dizziness, nausea and vomiting
Profuse Sweating
Management-
Remove the victim from the hot environment
Coding measures like cold spongy
Fluid replacement – by oral rehydration mixtures by IV saline
Monitor electrolytes and correct when needed.
Heat Syncope- Sudden loss of consciousness in a person with heat exhaustion due to combines effects of dehydration , prolonged peripheral vasodilatation and orthostatic pooling of blood in lower extremities .
Heat Stroke:-
- The most serious , life threatening form of heat related illness
- Provoked by a failure on the heat regulatory
- Mechanism of the body.
- Occurs in two forms-
– classic: without exertion, in people at risk.
– exertion: in the young engaged in rigorous exercise .
Symptoms’:- Headache, dizziness, weakness, confusion or euphoria is progressing into coma.
Hallucinations
Generalized seizures
Abrupt rise in body temperature(above 40C)
Management-
- Remove the patient from the hot area
- Cool with sponging and ice packs
- Manage in intensive care unit(Hypourlemia is often absent) .
Prevention of Heat disorders 6 Do’s 
- Do drink water even when you are not thirsty
- Do rest well before and on between exercise
- Do loosen your clothing while resting
- Do avoid strenuous exertion.
- Do rest in shade or use umbrella
- Do seek medical care if you are not feeling well.
7 RS in first aid
- Recognize the early signs and symptoms of heat related illness
- Rest the victim in a cool shady environment preferably in AC
- Resuscitate with CPR if the victim in unconscious
- Ring up the Ambulance services right away
- Reduce the body temperature as fast as possible by vigorously cold sponging .
- Rehydrate the victim , if he or she is conscious
- Rush the victim to the nearby hospital.
Dr. S Altaf Basha, MD
Professor & HOD Internal Medicine
GMCH& RC AJMAN





































